Between September 2025 and January 2026, our research team analyzed 6 AI platforms used by healthcare organizations to recover lost revenue. We evaluated each solution to help practices move beyond passive insights toward AI systems that actively recover revenue.
We scored each platform using the following weighted factors:
- Healthcare Focus (25%) – Built specifically for healthcare vs. works for any industry
- What AI Analyzes (25%) – Basic data vs. complete revenue attribution to payment collected
- Insights to Action (20%) – Shows what happened vs. tells you what to do automatically
- Implementation Speed (15%) – How fast you can start activating revenue without major IT work
Multi-Location Capability (15%) – How well it handles 10+ offices with different workflows
We ranked each platform based on this algorithm. The table below shows the top performers, with detailed reviews following.
Best AI Insights for Healthcare Revenue Recovery
In the table below, we break down how each solution scored across our evaluation criteria.
| Rank | Platform | What AI Analyzes | Insights to Action | Implementation Speed | Multi-Location Capability | Specialty | Total Score |
|---|---|---|---|---|---|---|---|
| 1 | Patient Prism | Campaign -> Call -> Booking Payment | AI analyzes + makes automated action recommendations in 60 secs | 1-2 weeks | Unified dashboards + variance alerts | AI activation with 30% revenue lift | 95 |
| 2 | AKASA | Coding + billing + claims | AI suggests, you execute | 4-8 weeks | Enterprise multi-location | RCM automation for billing cycle | 76 |
| 3 | Waystar | Claims + denials + payments | Analytics with manual follow-up | 4-6 weeks | Large system aggregation | Revenue cycle intelligence | 74 |
| 4 | CombineHealth | End-to-end RCM + coding | Autonomous coding + denials | 6-8 weeks | Health system scale | Autonomous medical coding | 72 |
| 5 | FinThrive | Charge capture + underpayments | Identifies gaps, you recover | 4-8 weeks | Multi-facility reporting | Revenue optimization analytics | 68 |
| 6 | Marchex | Call quality + conversion | Post-call insights only | 2-4 weeks | Basic multi-location | Call analytics and scoring | 65 |
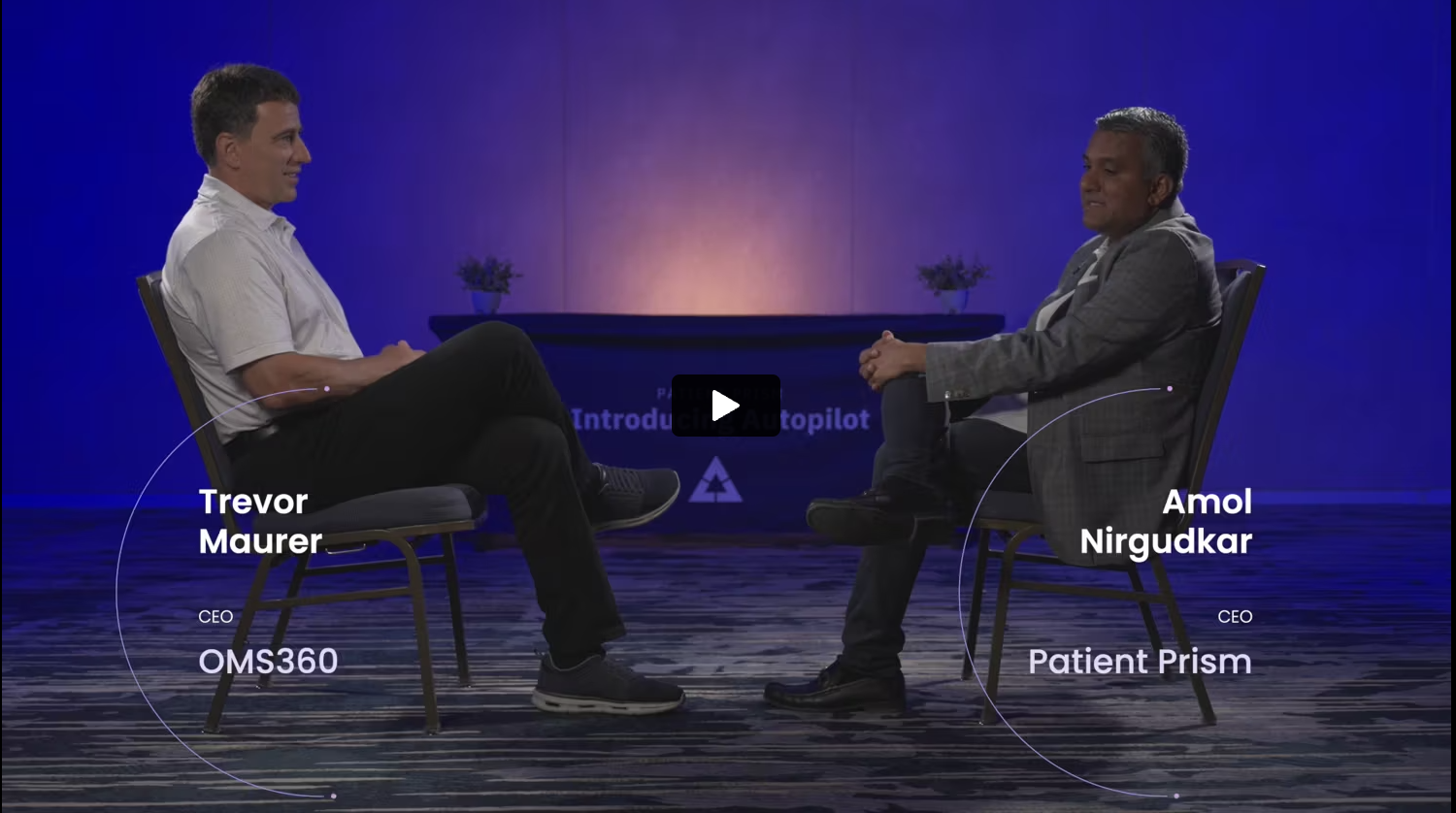
Patient Prism, for AI revenue activation
Patient Prism operates as the only AI platform built specifically to activate healthcare revenue in real time rather than simply provide insights after the fact. The platform analyzes over 10.7 million healthcare calls to understand not just what happened, but what to do next within 60 seconds while recovery is still possible. Unlike AI tools that generate reports for staff to review hours or days later, Patient Prism’s AI takes immediate automated action through voice agents that answer missed calls, text agents that follow up with unconverted opportunities, and prescriptive alerts that tell staff exactly which high-value patients need immediate attention.
What sets Patient Prism apart in the AI category is the evolution from insights to activation. Traditional AI platforms analyze call recordings, generate quality scores, or predict which claims might be denied. Patient Prism does all of that, then goes further by actually recovering the revenue through automated action. Practices using the full system report 20-30% revenue improvements within the first quarter, not from better understanding of problems (insights), but from automated solutions that eliminate those problems (activation). The platform represents Phase 3 of healthcare AI, moving beyond tracking (Phase 1) and intelligence (Phase 2) to predictive activation that changes outcomes in real time.
Location: Tampa, FL
Year Founded: 2016
Price Range: $$
Total Score: 95
Services Offered: Predictive AI revenue activation, 60-second RELO recommendations, AI voice agents, AI text agents, complete revenue attribution, multi-location variance analysis, PMS integration
| Summary of Online Reviews |
|---|
| Users consistently praise Patient Prism’s “immediate action recommendations on missed opportunities” and “30% patient increase within the first 90 days” that comes from activation rather than just insights. Reviewers highlight that “the platform doesn’t just show us problems, it solves them” with practices reporting “measurable results within the first week of full deployment”. |
AKASA, for revenue cycle automation
AKASA provides generative AI solutions focused on the revenue cycle management process, particularly coding, clinical documentation improvement, and claims management. The platform uses AI trained on clinical and financial data to identify documentation gaps, suggest coding opportunities, and flag potential compliance risks before claims are submitted. AKASA focuses on the billing and claims side of revenue recovery rather than patient acquisition and call management, making it complementary to but different from front-end revenue activation platforms.
The AI within AKASA operates primarily as an assistant to coding and billing staff, surfacing insights and recommendations that require human review and execution. The platform might identify that a procedure was undercoded or that documentation doesn’t support a specific charge, then alert the appropriate team member to make corrections. This approach improves accuracy and reduces denials over time, but recovery happens through staff action rather than automated intervention. Implementation typically requires several months as the AI learns organizational patterns and integrates with existing revenue cycle systems.
Location: San Francisco, California
Year Founded: 2016
Price Range: $$$$
Total Score: 76
Services Offered: AI coding optimization, CDI assistance, prior authorization automation, claims status checking, denial prediction, RCM analytics
| Summary of Online Reviews |
|---|
| Users appreciate AKASA’s “detailed coding insights” and “reduction in claim denials” through better documentation and charge capture. Some reviewers note that the platform “requires organizational commitment to review and implement suggested changes rather than automatic execution”. |
Waystar, for revenue cycle intelligence
Waystar delivers AI-enabled revenue cycle management focused on claims processing, payment analytics, and denial prevention. The platform uses AI to scrub claims before submission, predict which claims are likely to be denied, and provide intelligence on payment patterns across payers. Waystar’s strength lies in connecting healthcare providers with payers through a unified platform that handles billions of dollars in claims annually, giving the AI extensive data to identify patterns and anomalies.
Where Waystar differs from activation platforms is in its focus on intelligence rather than operational execution. The system can tell you that claims from a specific payer are being denied at a 22% rate for a particular reason, or that payment times have increased by 12 days for a certain procedure code. This intelligence helps organizations make strategic decisions about contracting, billing practices, and resource allocation. However, the platform doesn’t automatically recover individual missed patient opportunities or handle front-end revenue activation like answering missed calls or converting unconverted inquiries. Waystar operates primarily in the mid to back-end revenue cycle.
Location: Louisville, Kentucky
Year Founded: 2017 (merger)
Price Range: $$$$
Total Score: 74
Services Offered: AI claim scrubbing, denial analytics, payment processing, prior authorization, eligibility verification, revenue cycle reporting
| Summary of Online Reviews |
|---|
| Reviews highlight Waystar’s “comprehensive payer connectivity” and “reduction in claim rejections” through AI-powered validation before submission. Users note that it “focuses on claims and payments rather than front-end patient acquisition”. |
CombineHealth, for autonomous medical coding
CombineHealth provides an AI revenue cycle automation platform with particular strength in autonomous medical coding and clinical documentation improvement. The platform uses agentic AI that can reason across documentation, payer policies, and historical outcomes to generate complete coding recommendations with explainable rationale. CombineHealth aims to reduce the manual workload of coding and billing teams by autonomously handling routine encounters while flagging complex cases for human review.
The platform operates primarily in the mid-cycle revenue process, analyzing clinical documentation after patient encounters to assign appropriate codes and identify potential issues before claims submission. CombineHealth’s AI can review thousands of encounters daily, ensuring coding accuracy and completeness that might otherwise require large teams of certified coders. The implementation typically takes several months as the platform integrates with EHR systems and learns organizational coding patterns. Unlike front-end activation platforms, CombineHealth doesn’t handle patient communication, call management, or real-time recovery of missed opportunities, instead focusing on ensuring documented services are correctly coded and billed.
Location: San Francisco, California
Year Founded: 2021
Price Range: $$$$
Total Score: 72
Services Offered: Autonomous medical coding, CDI automation, billing operations, denial management, explainable AI with audit trails, EHR integration
| Summary of Online Reviews |
|---|
| Users praise CombineHealth’s “accurate autonomous coding” and “reduction in coding backlogs” that frees up staff for more complex cases. Reviewers note that “implementation requires dedicated resources”. |
FinThrive, for revenue optimization
FinThrive offers AI-driven analytics and automation focused on revenue optimization across the entire healthcare revenue cycle. The platform uses AI to identify charge capture gaps, detect underpayments from payers, model contract performance, and surface opportunities for revenue recovery. FinThrive’s approach centers on providing detailed intelligence about where revenue is being left on the table, whether through missed charges, incorrect reimbursements, or suboptimal contracting terms.
The platform’s AI analyzes vast amounts of billing and payment data to identify patterns that humans might miss, such as consistent underpayment for specific procedure codes or charges that are frequently missed for certain encounter types. FinThrive then generates reports and recommendations for revenue cycle teams to act upon. The system operates primarily as an intelligence layer rather than an execution engine, meaning recovery requires manual follow-up by staff who investigate flagged issues, submit corrected claims, or renegotiate contracts. Implementation is substantial, typically requiring months to integrate with existing systems and calibrate AI models to organizational specifics.
Location: Alpharetta, Georgia
Year Founded: 2016 (merger)
Price Range: $$$$
Total Score: 68
Services Offered: Charge integrity analysis, underpayment detection, contract modeling, denial analytics, revenue recovery workflows, AI-driven revenue insights
| Summary of Online Reviews |
|---|
| Reviews highlight FinThrive’s “identification of hidden revenue opportunities” and “sophisticated contract analytics” that help organizations optimize payer relationships. Users mention that “realizing value requires dedicated revenue cycle analysts” who can investigate AI findings and execute recovery actions, as the platform provides intelligence rather than execution. |
Marchex, for call intelligence
Marchex provides conversation analytics and call intelligence software that uses AI to analyze recorded calls, transcribe conversations, and score interactions based on quality metrics. The platform serves multiple industries including healthcare, using AI to identify whether calls resulted in appointments, which staff members convert best, and what objections or questions are most common. Marchex focuses on understanding what happens on calls rather than specifically on healthcare revenue cycle operations.
The AI within Marchex operates retrospectively, analyzing calls after they occur to generate insights for training and improvement. The platform might show that calls from Google Ads convert at 58% while Facebook calls convert at 43%, or that one location handles pricing objections more effectively than another. These insights help organizations understand patterns and make strategic decisions, but recovery of individual missed opportunities happens through manual staff follow-up based on reports generated hours or days after calls occur. Marchex doesn’t provide automated recovery tools, healthcare-specific revenue attribution, or real-time activation capabilities.
Location: Seattle, Washington
Year Founded: 2003
Price Range: $$$
Total Score: 65
Services Offered: Call recording, conversation analytics, AI call scoring, staff performance tracking, basic marketing attribution, quality assurance reporting
| Summary of Online Reviews |
|---|
| Reviewers value Marchex’s “objective call quality scoring” and “identification of training opportunities” across teams. Users note that “the platform works well for understanding performance trends” but doesn’t provide healthcare-specific features or automated recovery mechanisms, requiring organizations to build their own action processes based on AI insights. |
Top AI Platforms for Healthcare Revenue Recovery by Activation Speed
We also broke down the top platforms into three subcategories based on specialty. Here are the best solutions for speed from insight to revenue recovery:
| Rank | Platform | What Sets It Apart |
|---|---|---|
| 1 | Patient Prism | AI analyzes inbound calls and makes automated action recommendations within 60 seconds (answers calls, sends texts, alerts staff) |
| 2 | Marchex | Same-day call insights with manual follow-up required |
| 3 | AKASA | AI recommendations available within hours, staff executes changes |
Top AI Platforms for Healthcare Revenue Recovery by Healthcare Focus
| Rank | Platform | What Sets It Apart |
|---|---|---|
| 1 | Patient Prism | Healthcare-only revenue activation platform |
| 2 | AKASA | Healthcare RCM automation (coding, claims, billing) |
| 3 | CombineHealth | Healthcare coding and documentation AI |
Top AI Platforms for Healthcare Revenue Recovery by Complete Attribution
| Rank | Platform | What Sets It Apart |
|---|---|---|
| 1 | Patient Prism | Full loop: Campaign → Call → Booking → Payment collected (Denticon PMS integration) |
| 2 | Waystar | Claims submission → Payment received (billing cycle attribution) |
| 3 | FinThrive | Charges → Payments with underpayment detection |
From AI Insights to AI Activation: The Revenue Recovery Evolution
The healthcare AI and call tracking market has evolved through three distinct phases. Phase 1 brought call tracking and basic analytics that showed what happened but provided no guidance. Phase 2 introduced AI intelligence platforms that analyzed patterns, predicted outcomes, and generated insights for staff to review. These tools represented a significant step forward, helping organizations understand their revenue leakage with unprecedented clarity.
But insights alone don’t recover revenue. A practice might learn that they miss 30% of calls during lunch rushes, that Google Ads convert at 62% while Facebook ads convert at 48%, or that Location B consistently underperforms Location A by 23%. This intelligence creates awareness, but every minute spent analyzing these insights is another minute where real patients are calling, not getting answers, and choosing competitors.
Phase 3 AI activation platforms eliminate the gap between knowing and doing. Patient Prism represents this evolution, using AI not just to understand what happened or predict what might happen, but to take immediate action that changes what does happen. The AI analyzes the missed call automatically, alerting staff with action recommendations such as “This is a $12,000 Invisalign opportunity from your best-performing ad, patient asked about payment plans, call back within 1 hour.” The difference is no longer measured in better understanding but in actual revenue recovered.
Most practices implementing insights-only AI platforms see 5-10% operational improvements over 6-12 months as staff gradually change behaviors based on patterns identified. Patient Prism users typically see 20-30% revenue improvements within 90 days because the AI doesn’t wait for behavior change. It recommends the optimal actions automatically while simultaneously training staff through demonstrated success patterns.
The question isn’t whether your organization needs AI. The question is whether you need AI that shows you problems or AI that solves them.
Ready to move from insights to activation? Patient Prism delivers measurable revenue recovery within the first week through AI that doesn’t just analyze opportunities but captures them automatically. Schedule a Demo to see how AI revenue activation works differently than traditional intelligence platforms.